AI in Pricing, Reimbursement &
Market Access (PRMA)
by Michael Hurwich, SPG
AI in PRMA:
Where It’s Going
Artificial Intelligence (AI) has become more than just a buzzword. It is quickly transforming how the life sciences industry approaches Pricing, Reimbursement, and Market Access (PRMA). As regulations evolve and real-world data (RWD) become more robust, AI is helping companies make faster, smarter, and more evidence-based decisions about how to bring treatments to market and demonstrate their value to payers.
1) Evidence generation becomes AI-assisted by default
Health authorities such as the UK’s National Institute for Health and Care Excellence (NICE) are increasingly open to the use of AI in generating evidence, provided it is transparent, validated, and overseen by experts. AI tools can speed up processes that used to take months, such as reviewing thousands of research articles or extracting relevant data from clinical notes. (https://www.nice.org.uk/position-statements/use-of-ai-in-evidence-generation-nice-position-statement? )
This doesn’t replace human judgment. Instead, it allows teams to work more efficiently and with fewer errors. For example, AI can help with automated literature reviews, data extraction, and faster indirect treatment comparisons, allowing companies to build stronger evidence packages earlier.
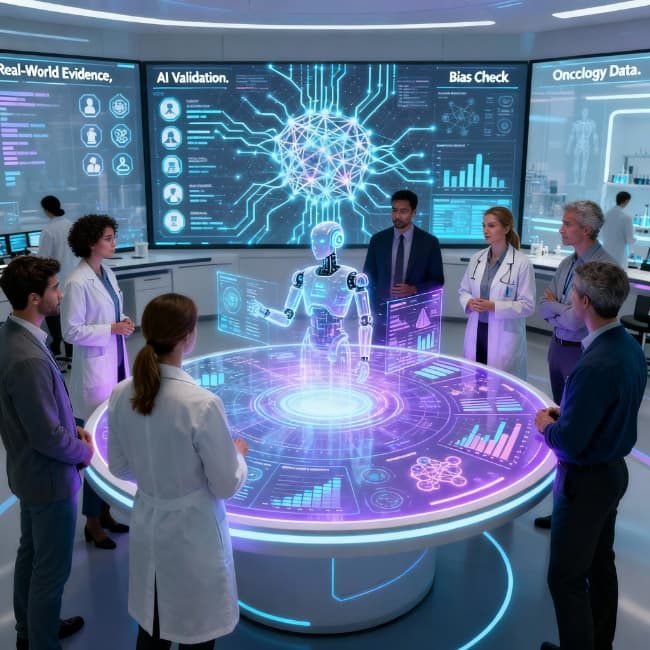
Driving smarter decisions in PRMA
Discover how AI accelerates evidence generation, optimizes pricing strategies, and strengthens payer partnerships. Embrace responsible innovation to achieve faster, more effective decisions in PRMA. Propel your future today with artificial intelligence.
These options capture the core message of AI transforming pricing, reimbursement, and market access, while inviting the reader to engage with this innovation responsibly.
